Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Advertisement
Nature Medicine (2023)
10
Metrics details
The COVID-19 pandemic stimulated an unprecedented push for digital transformation, accelerating the adoption of digital technology in health care1. There was a surge in telemedicine services, in artificial intelligence (AI) for SARS-CoV-2 detection2, and in the use of AI to predict blueprints for vaccine development3. With the increased digital flow of data, there is a need for privacy-preserving technologies to improve research and clinical applications within the healthcare system4,5. Data tokenization on the blockchain provides high levels of privacy and confers the potential for personal ownership of health data, which other privacy-preserving technologies such as federated learning and generative adversarial networks do not offer6,7,8 (see Table 1 for a glossary of terms). The use of non-fungible tokens (NFTs) is a potential data-management solution for the governance of data at both personal and institutional levels.
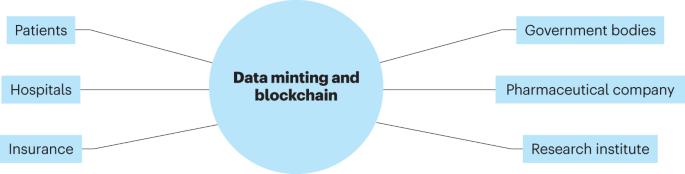
Tokenization is a data-security method and token types include platform tokens, utility tokens, governance tokens, security tokens, and NFTs. NFTs are supported on blockchain platforms such as Ethereum and Hyperledger Fabric, where each NFT is digitally unique. NFTs can be created via the minting of existing digital data, or they can use generative data, where the digital product is produced in whole or in part by an autonomous system. Once encoded with blockchain technology, a NFT cannot be modified, and its authenticity is validated through the blockchain in which it is stored. Hence, prior to minting, data must be cleaned, verified by verifiable credentials, and converted into an actionable form. This allows individuals to own and trade digital assets between parties such as multinational medical networks, pharmaceutical companies or insurance companies (Fig. 1).
A blockchain-enabled ‘biodata’ platform will serve as a decentralized and secure collaborative network for health data. This will enable the secure exchange of healthcare data among multiple stakeholders, including patients, hospitals, government bodies, pharmaceutical companies, research institutes and insurance companies.
We envisage several potential benefits of healthcare data tokenization in the form of NFTs. Ownership of data by patients may result in safer care by improving the fluidity of health information amongst different care providers. At present, rules around the protection of data privacy restrict the sharing of patient data across institutions, and inaccurate or incomplete information can result in misdiagnosis and suboptimal care. Patient access and ownership of data might overcome this situation. This increased fluidity of health information may render health economic benefits by reducing duplicate investigations or treatment.
Giving patients ownership and access to their health data might also encourage patient engagement in their care9, which can positively affect treatment compliance. Similarly, tokenization of health data allows patients to exercise autonomy over their own data, which could prevent companies from profiting from data aggregated via personal health applications, or unauthorized access to institutional databases by third parties who then sell sensitive health information. Instead, patients can actively choose to share personal data for research. This could address ongoing ethical concerns surrounding situations in which AI developers use publicly available patient data to develop AI algorithms that can be monetized, without the patients being financially rewarded.
Storing health data as NFTs can also ensure data authenticity by preventing modifications once data have undergone minting. Data integrity contributes to quality health care during clinical decision-making processes and will also contribute to more-accurate findings in research. The use of blockchain technology could also be used for drug verification to prevent counterfeit drugs. The use of smart contracts within NFTs further allows for reliable automation of data exchange. Smart contract is a rule-based algorithm that allows automated self-execution of the approval process when predetermined conditions or rules are met, which removes the need for human input in the execution process.
To tokenize health data, modifications must be made from existing NFT systems. We focus here on the minting process and less on the transactional nature of existing commercial NFTs. We propose that a blockchain ledger dedicated to healthcare data is identified or created, with tokenized data stored and verified, and where the data cannot be publicly viewed. This contrasts with existing commercial NFT marketplaces where the digital asset — such as an art or music file — can be publicly viewed, although owned only by the individual who generated or bought it.
A web-based or smartphone application could be created, in which each patient has a health wallet, similar to a cryptocurrency wallet, where tokenized digital health data can be accessed as NFTs via verifiable credentials. The health data to be tokenized must be characterized, which will involve determining whether the data are structured (such as laboratory values) or unstructured (such as radiology images and physician notes) and whether preprocessing of the data is required.
Once the infrastructure is ready, health data can be minted as NFTs. Acquired health data will undergo minting into a health NFT and made available in a patient’s health wallet. Patients will then have ownership and access to their own data and may subsequently decide whether to share or transfer ownership of these data to other parties in the network (Fig. 1).
Despite the potential benefits, however, there are barriers to the adoption of NFTs in health care. NFTs are susceptible to data security compromises owing to vulnerabilities with smart contracts. Stolen NFTs are not uncommon, as seen in the theft of Bored Ape Yacht Club NFTs, where hackers used phishing techniques to modify smart contracts. Moreover, tokenization of health data could lead to unethical exploitation, with patients being driven to participate in tests for monetary gains. In addition, the complexities of NFTs may pose a challenge for some people in terms of managing their own data.
Destruction of NFTs is possible and is done by ‘burning’ at present, with NFTs being sent to inaccessible addresses. However, NFTs are generally regarded as immutable and may exist on the blockchain forever, posing a challenge for the destruction or modification of any inaccuracies in health data that might compromise patient care and research integrity. The minting, transfer and storage of large amounts of healthcare data can also lead to high maintenance costs and power consumption, resulting in an enormous carbon footprint10. Minting of NFTs can vary in cost depending on the data size, transaction speed, blockchain utility fees, and data quality. The colossal amount of health data from the global population may be too much for existing infrastructure to support. The nascent technology of quantum computing may provide solutions for data storage, retrieval and analysis through quantum speedup and quantum supremacy. Future research to address these limitations and practical considerations will aid in the tokenization of health data.
NFTs in health care could revolutionize how sensitive health data are handled. At the heart of NFTs are transparency, accountability, privacy and patient autonomy — all of which are important values in health care. Further enhancements to safeguard data security and to simplify processes, as well as to increase accessibility to all, will be essential if NFTs are to start a revolution in digital health.
Ting, D. S. W. et al. Nat. Med. 26, 459–461 (2020).
Article CAS Google Scholar
Zhao, W. et al. Sci. Rep. 11, 14353 (2021).
Article CAS Google Scholar
Malone, B. et al. Sci. Rep. 10, 22375 (2020).
Article CAS Google Scholar
Mikk, K. A. et al. J. Am. Med. Assoc. 318, 1433–1434 (2017).
Article Google Scholar
Jensen, P. B. et al. Nat. Rev. Genet. 13, 395–405 (2012).
Article CAS Google Scholar
Sadilek, A. et al. NPJ Digit. Med. 4, 132 (2021).
Article Google Scholar
Venugopal, R. et al. Neural Netw. 153, 339–348 (2022).
Article Google Scholar
Ng, W. Y. et al. Lancet Digit. Health 3, e819–e829 (2021).
Article Google Scholar
Walker, D. M. et al. J. Am. Med. Inf. Assoc. 24, 1088–1094 (2017).
Article Google Scholar
Truby, J. et al. Energy Res. Social Sci. 99, 399–410 (2022).
Google Scholar
Download references
Singapore National Eye Center, Singapore Eye Research Institute, Singapore, Singapore
Zhen Ling Teo & Daniel Shu Wei Ting
Duke-NUS Medical School, National University of Singapore, Singapore, Singapore
Daniel Shu Wei Ting
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
Correspondence to Daniel Shu Wei Ting.
D.S.W.T. holds a patent on a deep-learning system for the detection of retinal diseases. D.S.W.T. is also a co-founder of, and holds equity in, EyRIS Singapore. Z.L.T. declares no conflict of interest.
Reprints and Permissions
Teo, Z.L., Ting, D.S.W. Non-fungible tokens for the management of health data. Nat Med (2023). https://doi.org/10.1038/s41591-022-02125-2
Download citation
Published: 23 January 2023
DOI: https://doi.org/10.1038/s41591-022-02125-2
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Advertisement
© 2023 Springer Nature Limited
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.